Wellness for a Lifetime
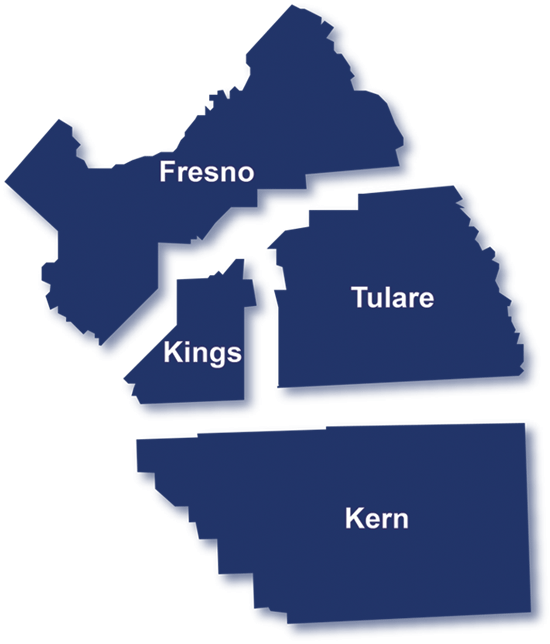
Serving over 100 communities in
Fresno, Kern, Kings, and Tulare Counties.
We are a premier health care provider
dedicated to your lifetime wellness.
We've Extended our Call Center Hours
Our call center is open until 9pm on weekdays and 8:30 am - 5:30 pm on the weekends.
"At United Health Centers, we are committed to doing everything we can for our patients." | Customer Service Pledge
800.492.4227
Schedule your appointment today.

Recognized as Top 10% Health Center Quality Leader by HRSA in 2023
United Health Centers soars into the top 10% of health centers to be recognized for our commitment to provide exceptional care in rural and underserved communities and the life-changing impact it can have.
Find us near you.
Locations
We are conveniently located to serve you best. Find premier healthcare near you.
Count on us.
Services
Serving you with excellent comprehensive health care services under one roof.

Need Medi-Cal or health insurance?
Enrollment Services
Our Enrollment Specialists are available to assist you with the Medi-Cal or health insurance enrollment process.

Work to make a difference.
Careers
We believe that every community deserves healthcare from caring and talented staff.

Over 30
Health Centers ready to serve you with more on the way


Providing over 50 years of
quality health care.
100+
California Central Valley communities where we serve as the premier health care provider


Top 10% Health Center Quality Leader by HRSA in 2023
UHC Highlights
Free Transportation - Now Available
We are now offering FREE transportation at our Hanford and Lemoore Health Centers.
Protect Your Family & Stay Healthy
United Health Centers has partnered with Kings County Public Health to offer you COVID-19 Testing, Vaccines, and Antiviral Medication Treatments.